What You Need to Know
There are 2 main types of medicine: over-the-counter and prescription medicine. Medicine that a doctor orders from a pharmacy is called prescription medicine. Over-the-counter (sometimes called OTC) medicine can be bought without a doctor's prescription. This doesn't mean that OTC medicines are harmless. Like prescription medicine, OTC medicines can be dangerous if not taken the right way.
Read on for more information from the American Academy of Pediatrics (AAP) about giving medicines safely to children and what to do if you think your child has swallowed any medicine or substance that might be harmful.
2. Read and Follow the Label Directions
Before you give your child any medicines, be sure you know how to use them. Check the label every time you give medicine to your child. If you need to give medicine at night, turn on the light to make sure you are giving the right medicine. If you have any questions about the medicine, ask your child's doctor, health care professional, or pharmacist.
For Over-the-counter Medicines
-
Check the box or bottle. Make sure it only treats the symptoms your child has.
-
Check the ingredients. Are the main ingredients ("active ingredients") of the medicine you are giving the same as the ingredients in other medicines your child is taking? It's important that you don't give your child too much of the same medicine. For example, acetaminophen is an ingredient in many OTC and prescription medicines, such as medicines for pain or fever and cough/cold medicines.
-
Check what age the medicine is for. You may need to contact your child's doctor first for certain ages, such as if your child is younger than 2 years.
-
Check the facts. Read the side of the medicine box or bottle (the part called "Drug Facts") and check the "Warnings" section.
-
Check the chart. Check the chart on the label to see how much medicine to give. If you know your child's weight, use that to help you see how much medicine to give. If not, use your child's age.
For Prescription Medicines
Be sure you understand how much, how often, and how long your child needs the medicine. If you have any questions, ask your child's doctor or pharmacist. For example, you may ask, "The instructions say to give the medicine 4 times a day. Does that mean every 6 hours? If yes, do I need to wake up my child in the middle of the night?" or "My child feels much better. Can I stop giving the medicine?"
4. Always Measure Liquid Medicines With the Right Dosing Tool
Liquid medicines must be measured carefully. Always use the dosing tool that comes with the medicine or that your child's doctor or pharmacist tells you to use. Never use teaspoons, tablespoons, or other household spoons to measure medicine.
Four types of dosing tools are available: droppers (for infants), syringes, dosing spoons, and medicine cups. The units of measure on a dosing tool may be marked "tsp," "tbsp," or "mL." One tsp (teaspoon) is equal to 5 mL (milliliters), and one tbsp (tablespoon) is equal to 15 mL (milliliters). To measure the right amount, make sure the number and unit for the dose of your child's medicine matches the number and unit on your dosing tool.
Types of Dosing Tools
 Dropper. In this example, a dropperful is the same as 0.8 mL.
Dropper. In this example, a dropperful is the same as 0.8 mL.

Syringe. 1 tsp is the same as 5 mL.

Dosing spoon. 1 tsp is the same as 5 mL.
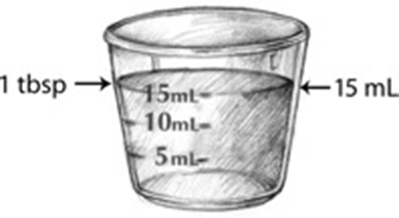
Medicine cup. 1 tbsp is the same as 15 mL.
What to Do for Poisoning
Sometimes parents find their child with something in his or her mouth or with an open bottle of medicine. If you think your child has swallowed any medicine or substance that might be harmful, stay calm and act fast.
-
Call 911 or your local emergency number right away if you cannot wake up your child (the child is unconscious), your child is not breathing, or your child is shaking (having convulsions or seizures).
-
Call 1-800-222-1222 (Poison Help) if your child is breathing and awake (conscious). A poison expert in your area is available 24 hours a day, 7 days a week. You will be told what to do for your child and whether you can watch your child at home or need to go to the hospital.
NOTE: You should not make a child throw up.
Listing of resources does not imply an endorsement by the American Academy of Pediatrics (AAP). The AAP is not responsible for the content of external resources. Information was current at the time of publication. The information contained in this publication should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Illustrations by Alex Anthony LeTourneau